Through evaluations and testing, the clinician will eliminate the possibilities of what disease process is occurring with the patient. Many diseases of the central nervous system present similarly to Autoimmune Encephalitis. As a complete diagnostic work-up is done, possibilities of the cause are ruled out. Infectious forms of encephalitis present similarly at onset to autoimmune encephalitis so a lumbar puncture is performed and testing is done in the cerebral spinal fluid (CSF) to rule out all possible infectious causes such as leading viral infections which include herpes simplex virus(HSV), Varicella-zoster virus (VZV), enterovirus, West Nile virus (WNV) and Japanese encephalitis (JE).
Once those possibilities have been excluded, bacterial causes are investigated and eliminated as possible culprits through testing spinal fluid. Bacterial causes of encephalitis include listeria, atypical presentations of streptococcus, syphilis, Lyme disease, and tuberculosis. Fungal causes such as Cryptococcus or aspergillis are particularly likely in immune compromised patients.
Due to the diversity of potential infections, recent research by Dr. Eric Lancaster at UPENN suggests advanced genetic techniques occur (e.g., metagenomic deep sequencing of cerebral spinal fluid) have been proposed to screen for thousands of pathogens rapidly and efficiently. This approach should assume a wider role in diagnosing unusual central nervous system (CNS) infections in the coming years. At this point in the investigation, the clinician has been able to rule out if the patient has a viral encephalitis or bacterial encephalitis and the investigation continues to determine if the patient could have autoimmune encephalitis.
What makes the diagnosis of autoimmune encephalitis unlikely (ruled out)? Time. If the patient doesn’t develop neurological symptoms within 4 weeks after onset of psychiatric symptoms, then the diagnosis of Autoimmune Encephalitis becomes very unlikely.
Next other medical causes are excluded some that present similarly to autoimmune encephalitis are Wernicke encephalitis, Intoxications such a neuroleptic malignant syndrome and serotonin syndrome, lymphoma or carcinomatous meningitis may present similarly to autoimmune encephalitis.
The syndromes that the patient presents with are clues to the clinician as to what is occurring as is the age and gender of the patient. For example, myoclonus (sudden, involuntary jerking of a muscle or group of muscles) can occur with the LGI1, DPPX antibody and the paraneoplastic antibody Anti-Ri (Anna 2).
At symptom presentation, about 80% of patients with autoimmune encephalitis have mild-to-moderate CSF lymphocytic pleocytosis (usually <100 white blood cells/μl), 30% have mild-to-moderate increase of protein concentration, and 50–60% have oligoclonal bands. These bands can be present even when routine CSF studies are normal. In contrast to most autoimmune encephalitis, the limbic encephalitis associated with LGI1-specific antibodies frequently occurs with normal or minimal CSF findings.
Diagnosis is confirmed through lab testing for antibodies known to cause these disorders, it is recommended that blood (serum) be tested at the same time as spinal fluid is tested. However some of these tests have been found to be less reliable than CSF testing. Cerebral spinal fluid (CSF) is 100% sensitive and 100% specific when testing for NMDA, for example, where blood or serum testing can give a false reading as the sensitivity of finding Anti-NDMA antibodies in serum is only ~75% with a 97%+ specificity. This means you may miss about 25% of cases. So, if there is a high index of suspicion, even if the serum test is negative, a CSF sample should be acquired and evaluated.
Other testing: Magnetic resonance imaging, MRI of the brain with and without contrast for abnormalities suggestive of autoimmune encephalitis is very useful in patients with limbic encephalitis, usually showing increased FLAIR/T2 signal involving one or both temporal lobes. It is possible that the MRI may be read as normal. FDG-PET is suggested to be more sensitive than MRI and 18fluorodeoxyglucose (18F-FDG) PET imaging has been reported to typically reveal medial temporal lobe hypermetabolism even in MRI-negative or inconclusive cases. The FDG-Pet is particularly important for patients with limbic encephalitis who often have normal or non-specific MRI findings. EEG (often sleep deprived so the neurologist can see how your brain is functioning when it is tired or a 24 hour EEG) possibilities include: low wave activity in temporal lobes, or diffuse slowing, epileptic activity or extreme delta brush pattern. Any one of these are a possible finding of evidence. Cat scan may be performed for a tumor search, Lumbar puncture for any signs of inflammation or disease in the central nervous system.
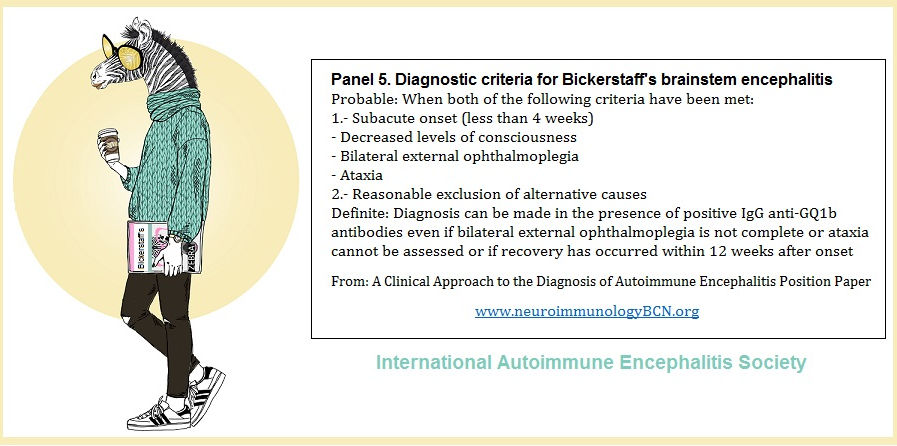
The ground breaking position paper, A clinical approach to diagnosis of autoimmune encephalitis was a collaborative work by some of the most renown medical researchers and clinician in the field of Autoimmune Encephalitis today. It was published in the Lancet in February 2016 and outlined how to diagnose autoimmune encephalitis with the technology available in all general hospitals and NOT to wait to treat until the antibody test results have come back. Best outcomes are achieved when treatment is begun immediately and antibody test results can take 7 to 10 days to receive.
*Every Medical practitioner who may one day see a patient with autoimmune encephalitis: Neuroimmunologists, Neurologist, Immunologists, Psychiatrists, Rheumatologists, Endocrinologists, Emergency Department physicians and medical students should be aware of this paper.
The experts on this paper are:
Francesc Graus, Maarten J Titulaer, Ramani Balu, Susanne Benseler, Christian G Bien, Tania Cellucci, Irene Cortese, Russell C Dale, Jeff rey M Gelfand, Michael Geschwind, Carol A Glaser, Jerome Honnorat, Romana Höftberger, Takahiro Iizuka, Sarosh R Irani, Eric Lancaster, Frank Leypoldt, Harald Prüss, Alexander Rae-Grant, Markus Reindl, Myrna R Rosenfeld, Kevin Rostásy, Albert Saiz, Arun Venkatesan, Angela Vincent, Klaus-Peter Wandinger, Patrick Waters, Josep Dalmau
When should the clinician suspect an Autoimmune Encephalitic Disorder?
If the patient is presenting with rapidly progressive encephalopathy of unclear etiology they will most often have multi-focal symptoms. Pure symptoms of just abnormal movement or just psychosis is rarely seen. They can present like this but usually the progression is rapid and multiple neurological are present. Inflammatory findings in the Central spinal fluid (CSF) such as mild to moderate pleocytosis and oligoclonal bands can be present when routine studies are negative. This is supportive of an inflammatory autoimmune process. It doesn’t give you a diagnosis as a viral process and other disorders can have this finding but it is a piece of evidence. In some cases, the MRI can be helpful. MRI with FLAIR-T2 changes in hippopotamus are seen in LGI1, GABA (B), and AMPA. If you have a bilateral medial temporal lobe flair signal and the viral studies are negative, it is not necessary to have an identified antibody to start treatment. The doctor should begin treatment at that time. - Dr. Josep Dalmau
The development of extrapyramidal symptoms (EPS) when placed on antipsychotics should alert the team to consider this diagnosis. Of course, EPS is a known side effect of antipsychotics anyways, but it just another reminder to consider the possibility of Autoimmune Encephalitis. A new onset of possible Neuroleptic Malignant Syndrome should also make the team consider the possibility of Autoimmune Encephalitis (especially if the Creatine Kinase (CK) is normal, or CK normalizes after treatment, but without improvement.)
Encephalopathy, Autoimmune Evaluation, Serum Antibody Testing
Encephalopathy, Autoimmune Evaluation, Spinal Fluid Antibody Testing
Lancet Podcast Clinical Approach to Diagnois of Autoimmune Encephalitis

How is Autoimmune Encephalitis diagnosed?
Diagnosis




International Autoimmune Encephalitis Society, Inc. IAE Society is a Delaware Charitable foundation and a registered 501(c)(3) organization.
International Autoimmune Encephalitis Society
Empowering victims of Autoimmune Encephalitis and caregivers through Support and Education

Chart of Causes of Encephalitis that are not autoimmune From Diagnosis and Treatment of Autoimmune Encephalitis.
These possibilities are ruled out by testing of spinal fluid. If the patient is negative for encephaltis, testing for identified antibodies in Autoimmune encephalitis is done to find the cause of the illness and help to arrive at a diagnosis.






This article reviews how a diagnosis is arrived at and that the existence of Ab-negative autoimmune encephalitis was supported by the finding that 44% of patients that are rituximab responders have autoimmune encephalitis without detectable antibodies. FDG-PET is sometimes useful as a diagnostic tool in patients with a normal MRI, and exhibit medial temporal hypo- or hypermetabolism and basal ganglia hypermetabolism in anti-LGI1 encephalitis.
Andrew McKeon, M.B., B.Ch., M.D., Mayo Clinic Webinar: The Spectrum of Autoimmune CNS Disorders 1 hour 11 minutes June- 2017
Intended Audience
This webinar is designed for any provider who sees patients with a neurologic disease (e.g., neurologists, psychiatrists, primary care physicians including internists and family care practitioners) as well as pathologists, laboratory directors, and laboratory sendout coordinators.


