When Dr. Josep Dalmau identified the first antibody, NMDAr, in 2005, that marked the beginning of the molecular identification and understanding of these autoimmune encephalitic disorders. At this writing, there are 16 types of autoimmune encephaladies disorders that have been identified.
There are multiple types of antibodies in Autoimmune Encephalitis. They have different clinical presentations and syndromes and have different responses to treatment. We know from the immunology world that antibodies come in many shapes and forms. There is a growing list of antibodies in each category. Autoimmune encephalitis may be divided into several groups of diseases: Those antibodies that can access the cell surface of an antibody or the synaptic receptor of an antibody that is accessible to the targeting antibody because it is exposed on the outside. Cytoxic T-cell diseases associated with antibodies to intracellular antigens, and those associated with other autoimmune disorders.
Extracellular antibodies target the receptor on the outside surface of the cell. There, it binds to the receptor on the outside surface of the healthy neuronal cell.
As more cases appeared, and neuronal targets could not be identified, that lead researchers to discover that the unknown cell surface antigens were not cell surface antigens at all, but in fact were found to be synaptic receptors, including the N-methyl-D-aspartate receptor (NMDAR). This discovery led investigators to distinguish a new category of autoimmune encephalitis those where the offending antibody is actually targeting the synaptic receptors in the brain.
In the disorders investigated so far that occur with autoimmune encephalitis, researchers who have studied their underlying mechanisms have seen that the antibodies alter the structure or function of the antigen they have targeted and bonded too. This attacking antibody that the immune system has created, now causes the antibody it has attached itself to, to malfunction or die.
These attacks can occur throughout the brain. Symptoms wax and wane (come and go in severity) as the attacks occur. At times, some symptoms may be more dominate and not so severe at other times. This is due to the fact that different areas of the brain may be under attack at different times. It is the fluctuation of symptoms and the vast array of symptoms the patient is experiencing that causes the neurologist unfamiliar with these disorders to fail in arriving at an accurate and timely diagnosis. This is a key reason we advocate that those suffering from Autoimmune Encephalitis hire a top expert in the field who has published on the disease as experience bares out that this leads to correct diagnosis and accurate, aggressive treatment that leads to best outcomes.
Viral disorders can trigger synaptic Autoimmunity~
The one instance where research has proven that patients can experience a virus triggering synaptic autoimmunity is in the case of herpes simplex virus. The patient who first has herpes encephalitis may a few weeks later come back to the hospital with what used to be called “choreathetosis HSV” and was thought to be a relapse. Now it has been identified that most of these patients have an autoimmune encephalitis mediated by the NMDA receptor. When they had herpes encephalitis, they did not have the NMDA antibody, yet a few weeks later when what looks like a relapse is occurring, it is identified that the patient now has NMDA receptor Autoimmune encephalitis. The virus triggered the change and research has yet to determine if it is due to molecular mimicry or perhaps by the inflammation, destruction and presentation of the antigen.
Dr. Dalmau discussing his paper on
Herpes Simplex Virus >NMDAr AE
Overlapping Immune Responses~
Although it is not common, sometimes more than one antibody may be occurring. NMDAr may occur with AQP4 or MOG antibodies. These patients have NMDAr autoimmune encephalitis and Neuromyelitis Optica spectrum disorder (NMO/NMOSD). NMDAr may occur with demyelinating disorders seen clinically and/or MRI demyelination in a study by Dr. M. Titulaer, February-11-2014.

Antibody testing~
Autoantibody testing is extremely important for the proper diagnosis of autoimmune encephalitis. In the correct clinical context, these antibodies can be diagnostic. However, the tests have complexities that require consideration, and taking certain test results as conclusive evidence of autoimmune encephalitis can be a mistake.
NMDAr and other cell surface antibody tests are most sensitive and specific with CSF. Serum may offer a low false positive rate and a higher false negative rate. Commercial tests for autoantibodies to NMDAR, LGI1, Caspr2, AMPAR (GluR1, GluR2 subunits), and GABA-B-R are widely available. Newer cell surface antigens like GABAA-R and DPPX are more difficult to test clinically. Have your physician contact Mayo Clinic Rochester, MN to inquire about antibody testing through research resources.
It is important that the doctor be comprehensive and test both the serum and the Cerebral spinal fluid (CSF) because of false positives with these antibodies. The antibodies are very helpful in making the diagnosis but following the titers of these antibodies should not guide the doctor in making clinical decisions. Patients tend to recover despite having a level of antibodies. Dr. Dalmau recommends that doctors think about the way this is seen in myasthenia gravis.
*Laboratories that perform antibody testing is listed under Resource Section
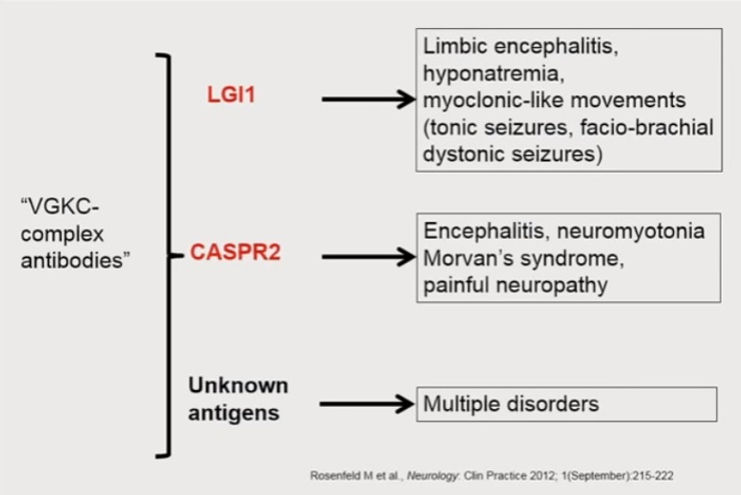
Caspr2 and LGI1 each associate with VGKCs
Before 2007 when Dr. Dalmau identified the first antibody in autoimmune encephalitis, the only cell-surface antibodies associated with autoimmune encephalitis (limbic encephalitis and Morvan’s syndrome) were attributed to antibodies specific for the Kv1.1 and Kv1.2 subunits of the Shaker family of voltage-gated potassium channels (VGKCs). This was later shown to be wrong.
The VGKC antibody test is based on immunoprecipitation of a complex of protein containing VGKCs, LGI1, Caspr2 and other proteins. For 15 years, before the LGI1 and Casper2 antibodies were recognized, patients with VGKC antibodies were thought, incorrectly, to actually have antibodies to potassium channel subunits themselves. The VGKC test may still detect patients with LGI1 or Caspr2 immunity, but low titer serum positive results have uncertain clinical significance. For instance, Paterson et al. reported that only 4 of 32 patients with low titer VGKC results (100-400 pM) actually had an autoimmune disorder. Therefore, a low titer serum VGKC result without corresponding evidence of LGI1 or Caspr2 antibodies, ideally in the CSF, should not be taken as definitive evidence of autoimmune encephalitis.
Dr. Josep Dalmau in his September 2016 presentation on autoimmune encephalitis at the AAN talked about the importance of specifying the type of molecular target as either LGI1 or CASPR2. If these impressions are negative for these 2 antibodies, and the VGKC are positive, you really don’t know what you are dealing with, he explained. When they get some of these cases to qualify, it has been found that they do not react at all with the cell surface. They are not against the potassium channels and researchers really don’t know what it is. Presently, there has been increasing interest in the VGKC patients without LGI1/Caspr2 antibodies questioning its relevance in clinical practice. These cases can be associated with many foreign disorders. Although the percentage is much lower proportionally, positive VGKC levels can be seen in normal individuals.
To summarize: Anti-LGI1 encephalitis and anti-Caspr2 encephalitis are separate clinical entities. Early recognition and treatment is necessary and rewarding. The term VGKC-complex antibodies, lumping patients with anti-LGI1, anti-Caspr2 antibodies or lacking both, should be considered obsolete.
Clinicians are told to be careful that they specify either LGI1 or CASPR2 and these are associated with specific types of syndromes as seen in the chart below.
Antibody Associated Paraneoplastic Disorders in AE


Antibodies in
Autoimmune Encephalitis
Cell Surface & Synaptic Proteins
International Autoimmune Encephalitis Society, Inc. IAE Society is a Delaware Charitable foundation and a registered 501(c)(3) organization.

Dr. Josep Dalmau presents at the AAN conference Sept 2016 : "Autoimmune Encephalitis the cell surface and synaptic antibodies"


